Mpox virus (formerly monkeypox) is making a worrying comeback across West and Central Africa, with Sierra Leone now at the center of a fast-growing outbreak. Despite past experiences with the virus, the scale and speed of the 2025 Mpox outbreak in Sierra Leone is raising alarm among global health leaders, putting hard-earned lessons from Ebola and COVID-19 to the test.
Mpox Resurgence in Africa: Why Sierra Leone Is in the Spotlight
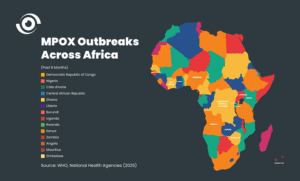
As of June 16, 2025, Sierra Leone’s National Public Health Agency reported 4,085 confirmed Mpox cases and 25 deaths, making it the third most affected country in Africa this year—after the Democratic Republic of the Congo (DRC) and Uganda.
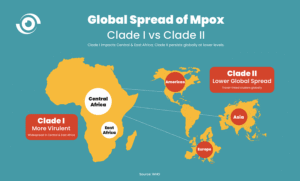
This follows a severe Mpox outbreak in DRC in 2024, which triggered a Public Health Emergency of International Concern (PHEIC) and a Public Health Emergency of Continental Concern (PHECS). Mpox cases are now being reported in several African countries, including Togo, Ghana, and Liberia, highlighting the virus’s potential to spread regionally.
How Mpox Spreads and Why It’s Hard to Control
Mpox spreads primarily through close contact, including skin-to-skin or intimate interaction. Once community transmission is established, it becomes difficult to contain—especially without:
Early detection systems
Strong health communication
Mass vaccination programs
Public trust in health authorities
Inside Sierra Leone’s Response to the Mpox Outbreak
Despite limited resources, Sierra Leone has launched a multi-pronged public health response, led by Health Minister Dr. Austin Demby and supported by the newly formed National Public Health Agency. Key efforts include:
Activation of a Level 2 health emergency
Establishment of Mpox treatment centers, including a 50-bed MSF-supported facility in Calaba Town
Surveillance and contact tracing: over 5,900 contacts traced, with 4,200 completing monitoring
Public education via radio, mosques, schools, and community leaders
Health worker training and IPC (Infection Prevention and Control) measures
However, authorities report challenges such as low treatment center compliance, insufficient funding, and vaccine shortages.
Vaccine Supply Challenges and Cost Barriers
Sierra Leone received 61,300 Mpox vaccine doses from GAVI’s emergency stockpile, prioritizing healthcare workers and high-risk communities. But these have been exhausted. With vaccine prices exceeding $100 per person, national-scale vaccination is unaffordable without external funding—posing a major public health risk.
Mpox in West Africa: A Growing Regional Threat
Beyond Sierra Leone, other West African countries are now reporting rising Mpox cases:
Togo: 8 cases (as of June 12)
Ghana: 79 cumulative cases (as of June 10)
Liberia: 66 cases (as of June 9)
This rising trend signals regional transmission and the urgent need for cross-border collaboration. Health systems across West Africa remain vulnerable without coordinated strategies.
Role of WAHO and Regional Public Health Institutions
This outbreak presents a crucial opportunity for the West African Health Organisation (WAHO) and the Regional Centre for Surveillance and Disease Control (RCSDC) in Abuja to take regional leadership. Here’s how:
1. Regional Coordination and Support
WAHO can support joint vaccine procurement, resource distribution, and policy alignment across ECOWAS member states.
2. Emergency High-Level Advocacy
WAHO must lead efforts to engage ECOWAS, the African Union (AU), GAVI, and international partners to secure technical support and emergency funding.
3. Hosting a Regional Health Summit
WAHO and RCSDC can convene ministers of health, national public health leaders, and development partners to design a regional Mpox response plan.
4. Strengthening Health Systems
This Mpox outbreak is a call to invest in epidemic preparedness, laboratory networks, early warning systems, and public health workforce development across West Africa.